Peter J FIoramonti, United States
SUNY Upstate Medical University
Conversion to Belatacept in Kidney Transplant Recipients
Mahmoudreza Moein1, Benson Li1, Peter Fioramonti 1, Rauf Shahbazov1, Samir Iskhagi1, Matthew Hanlon1, Reeba Thankachan1, Christine Yang1, Reza Saidi1.
1Surgery/ Transplantation services, SUNY Upstate Medical University, Syracuse, NY, United States
Background: The costimulatory inhibitor Belatacept (Bela) has been shown to be an effective alternative as a post-kidney transplant immunosuppressant. This study focused on the outcome of early vs. late conversion to the Belatacept.
Material and Method: We conducted a retrospective analysis of a prospectively collected database of all kidney transplants adult patients at SUNY Upstate Medical Hospital from 1 January 2014 to 1 December 2022. . The early conversion was defined as all conversions done at < 6 months after kidney transplant, and Late conversion to Belatacept was defined as conversion at > 6 months post-transplantation.
Results: 61 patients were included in the study and divided into early and late conversion to Belatacept groups. 33 patients (54%) were in the early conversion group, and 28 patients (46%) were in the late conversion group. The mean eGFR was 26.73 before conversion to the Belatacept in the early conversion group, which improved over one year of follow-up with the mean eGFR of 45.3 at one year (P=0.0006). eGFR changes were insignificant in the late conversion group, in which the mean eGFR was 46.30 before conversion to the Belatacept, and it was 44.76 after one year of follow-up and stabilized (P=0.72).
7 allograft biopsy-proven rejection episodes were diagnosed overall, 4 episodes (57.1%) in the early conversion group and 3 episodes (42.9%) in the late conversion group. In 6 episodes (85.7%), patients did not have Tacrolimus in their immunosuppression regimen with Belatacept. However, when we analyzed the whole sample, we did not mention a significant difference in the rejection rate when Tacrolimus was part of the immunosuppressive regimen (P=0.6). All 4 biopsy-proven allograft rejections in the early conversion group were acute T-cell-mediated rejections. In the late conversion group, from 3 biopsy-proven rejections, 1 was chronic antibody-mediated rejection (CAMR), 1 T-cell-mediated rejection, and 1 was mixed antibody-mediated and T-cell-mediated rejection.
Surprisingly, in all 4 T-cell-mediated rejections (100%) in the early conversion group and, the one T-cell-mediated rejection in the late conversion group, mycophenolic acid (MPA) was part of the patient’s immunosuppressive regimen.
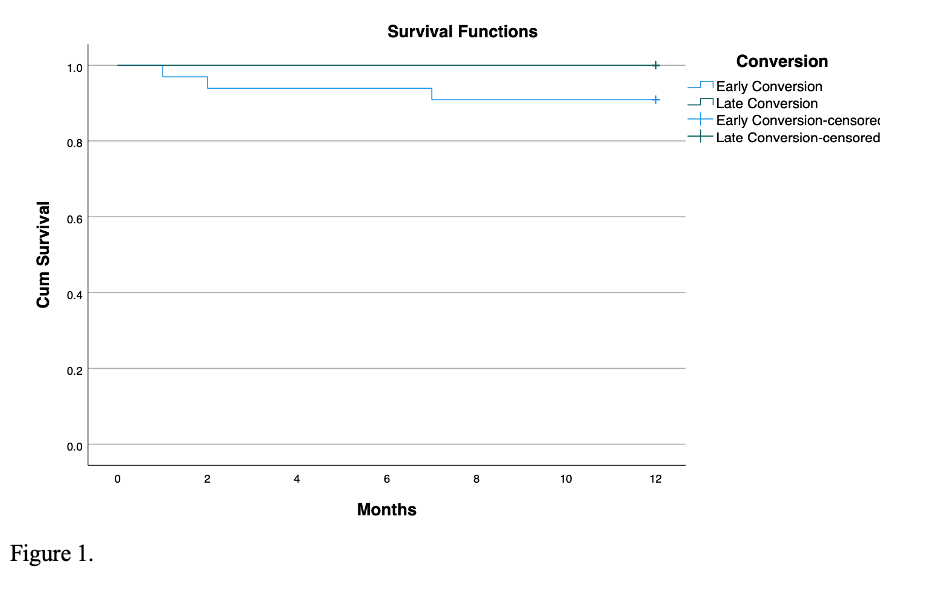
The one-year post-conversion allograft survival rate in both groups was 100%. The one-year post-conversion patient survival rate was 90.9% in the early conversion group and 100% in the late conversion group (P=0.11, Fig 1).
Conclusions: We conclude that early conversion to the Belatacept can significantly improve the eGFR compared to the late conversion. Belatacept and MPA without Tacrolimus might increase the chance of T-cell-mediated rejection.
Lectures by Peter J FIoramonti
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Tue-02 11:00 - 12:30 |
Patient Perspectives | Immunosuppression minimization during COVID infection: is it safe? | Grand Georgian |
|
Wed-03 10:30 - 11:00 |
Abstracts Session 7 | Conversion to Belatacept in Kidney Transplant Recipients | Grand Georgian |
