Master's Candidate
Pathology and Laboratory Medicine
University of Western Ontario
The role of DLC1 beta in attenuating cardiac ischemia-reperfusion injury during heterotopic heart transplantation
Samantha Collings1,6, Wei-Ping Min1,2,3,4,6, Xiufen Zheng1,2,3,4,6, Qi Liu1,6, Shun-Cheng Li5, Rakesh Joshi6, Hong Diao6, Danielle Taray-Matheson1,6, Sohyun Won1.
1Pathology and Laboratory Medicine, University of Western Ontario, London, ON, Canada; 2Department of Microbiology and Immunology, University of Western Ontario, London, ON, Canada; 3Surgery, University of Western Ontario, London, ON, Canada; 4Department of Oncology, University of Western Ontario, London, ON, Canada; 5Biochemistry, University of Western Ontario, London, ON, Canada; 6Matthew Mailing Centre for Translational Transplantation Studies, Lawson Health Research Institute, London, ON, Canada
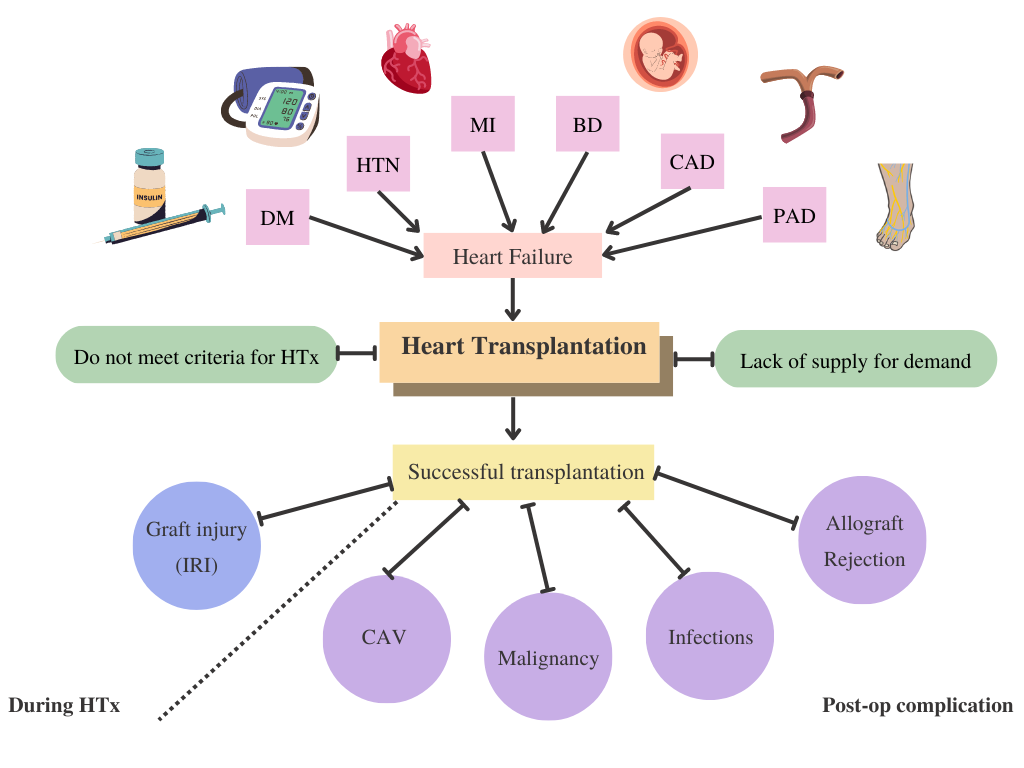
Introduction: Heart failure (HF) occurs when the heart becomes hemodynamically impaired; and is a prevalent disease with a significant associated morbidity/mortality. Currently, the only curative treatment for HF is heart transplantation (HTx). However, many grafts are affected by cardiac ischemia-reperfusion injury (IRI) during the process of HTx. IRI grafts display myocardial hypertrophy, de-regulated angiogenesis, and increased apoptotic cell bodies. Currently, the pathogenesis of cardiac IRI remains elusive. Past research displayed evidence that the PI3K/Akt & RhoA/ROCK pathways may attenuate cardiac IRI. Therefore, a beta-isoform of deleted-in-liver cancer protein 1 (DLC1β) that regulates Akt transcripts/RhoA activity is of interest to investigate further. It is hypothesized that DLC1β overexpression attenuates cardiac IRI by abrogating apoptotic injury via the RhoA/ROCK & PI3K/Akt pathways. It is predicted that overexpressing DLC1β by transfecting with a DLC1β overexpression (OE) plasmid would highlight potential cardioprotective effects during cardiac IRI.
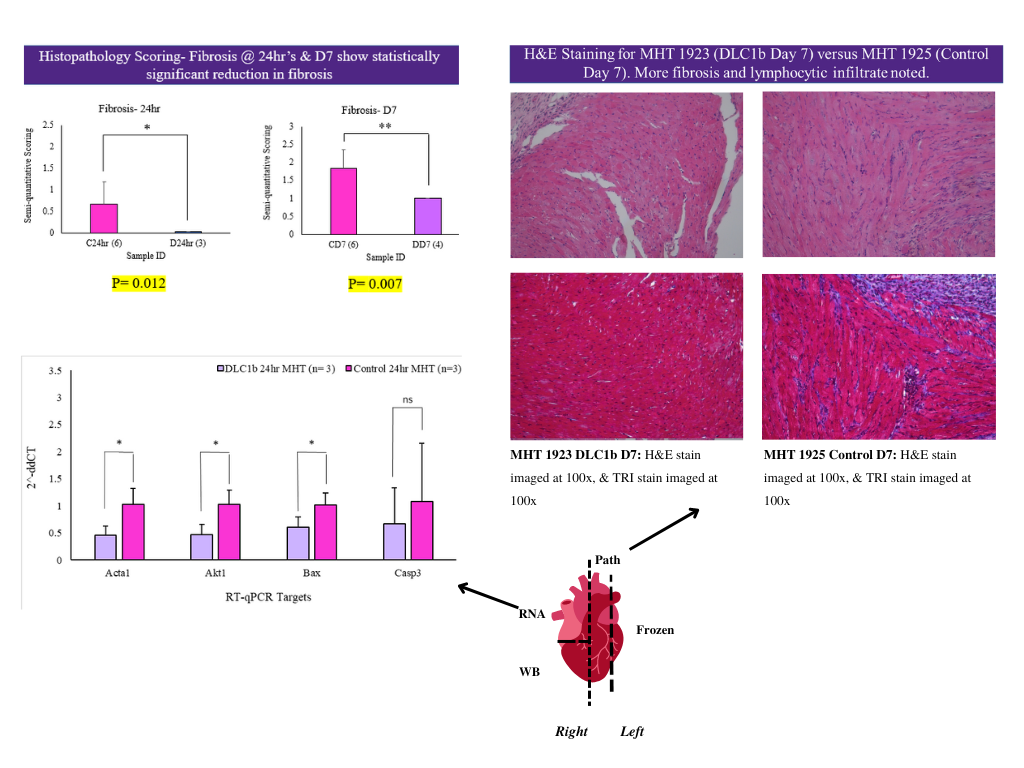
Methods: An in-vitro design utilizing H9C2 (rat cardiomyocyte), and HL-1 (mouse atrial cardiomyocyte) cell lines was performed using anaerobic respirators (GENbag's) and hypoxia-oxygenation reperfusion chambers (H/OR). Cells were then transfected with DLC1β OE plasmid/pc3 plasmid (control)/ or transfection medium (blank) and collected for further analyses (Western blot/RT-qPCR/cell viability assays, etcetera). Additionally, the study included an in-vivo mouse abdominal heterotopic HTx (MHT) model using wild-type C57/BL6 male mice. MHT’s were performed on three groups (wild-type (blank) mice, control mice (pc3 transfected), and DLC1β OE mice). Donors received tail-vein injections 24hrs pre-MHT before being sacrificed (sac'd). Grafts were stored at 4°C in UW solution for 24hrs, before being transplanted into syngeneic recipients. Recipient mice were sac'd 24hrs/7days post-MHT. Harvested grafts were analyses with histopathology, western blot, RT-qPCR, etc.
Results: In-vitro, there appears to be less early/late apoptosis when transfected with DLC1β OE plasmid compared to control groups noted on Annexin V flow cytometry assays. There also appeared to be a significant reduction in cell death via Incucyte SYTOX analyses in DLC1β OE groups. In-vivo, there appears to be a reduction in semi-quantitative injury grade noted in histopathological analyses when DLC1β is overexpressed. However, further analyses are required to reduce intragroup variability and for further pathway analyses.
Conclusion: It is of interest to further analyze the potential cardioprotective effects of DLC1β for future therapeutics. It’s expected that DLC1β is anti-apoptotic, and downregulation during cardiac IRI contributes to the extent of injury seen. Findings of this experiment are believed to be significant to the field, as reducing cardiac IRI could potentially enhance transplant efficacy and research recapitulation.
Heart and Stroke Foundation of Canada.
Lectures by Samantha L Collings
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Tue-02 09:20 - 10:30 |
Abstracts Session 3 | The role of DLC1 beta in attenuating cardiac ischemia-reperfusion injury during heterotopic heart transplantation | Grand Georgian |
